News from The Open University

On World Book Day find out how the OU’s Reading Schools Programme is helping more children to read for pleasure
Today is World Book Day and as children around the world excitedly mark the occasion by dressing up as their favourite literary character, or join in with special events at…
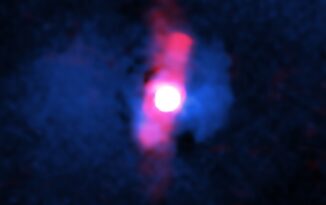
Students use NASA telescope to identify an underachieving black hole
An international team of students, including a PhD student from The Open University (OU) have revealed that a brilliant supermassive black hole is not living up to expectations in a…

500 ‘diagnostic’ assessments!? Time to reflect
Let me start with a story. Many years ago, I had a student who was struggling to get specialist support to meet his learning needs. He had dyslexia and was…

Employers report a values and skills mismatch with younger workers
Three in four (72%) of employers have seen a shift in young people’s (16-24-year olds) values and priorities in the workplace in the past three years, with over half (51%)…

Disabled veteran’s life-changing journey and his bid to help others
Dan Richards is a disabled veteran whose life was turned around thanks to an Open…

OU Alum Sir David Harrison, one of Universities UK’s 100 faces campaign
Sir David Harrison, MBA alumnus and Honorary Graduate of The Open University has been named…























